The other targets of alcohol use disorder
The systemic effects of alcohol abuse

Drinking alcohol is an established and normalised practice in our society, even though it can physically harm us. High-risk alcohol drinking patterns can increase the chance of negative consequences for the drinkers or their environment. The liver is by far the organ most affected by alcohol abuse; however, alcohol use disorder is a systemic disease which affects a wide range of organs and psychological processes. Other systems that can be affected by continued alcohol consumption include the immune, neurological, and cardiovascular systems. In addition, alcohol can lead to epigenetic alterations that may be transmitted from one generation to the next.
Keywords: alcohol use disorder, immunity, neurological damage, cardiovascular system, epigenetics.
Alcohol consumption is here to stay and has been normalised in our culture and society. In fact, alcohol use has been hegemonic among addictive substances throughout human history. Indeed, palaeogenetics, an emerging field that seeks to examine the protein predecessors preserved in the remains of ancient organisms, was able to trace an alcohol dehydrogenase class 4 (ADH4) mutation (the first digestive-tract enzyme capable of metabolising ethanol) to primates dating back approximately ten million years (Carrigan et al., 2015).
According to the latest report by the Spanish Observatory on Drugs and Addictions, alcohol is, without a doubt, the most widely consumed psychoactive substance in the Spanish population and the one responsible for the highest number of treatment admissions for abuse or dependence on legal or illegal substances. More specifically, around 25,000 admissions for the treatment of alcohol use disorder (35 % of all substance-use admissions) are registered annually in Spain. Moreover, the substance is also present in most patterns of polydrug use, especially for cocaine and cannabis (Observatorio Español de las Drogas y las Adicciones, 2020).
«Alcohol is the most widely consumed psychoactive substance and is responsible for the highest number of admissions for abuse or dependence treatment»
High-risk alcohol drinking patterns can increase the chance of negative consequences for the drinkers and their environment. Indeed, different forms of excessive alcohol consumption can pose a health risk or cause significant harm to the individual. These include heavy weekly or daily drinking, acute episodes of alcohol intoxication, and binge drinking (consuming five or more alcoholic drinks in a short period of time).
The prevalence of high-risk alcohol consumption in the Spanish population aged 15–64 years, measured through AUDIT, stands at 5.1 %, allowing us to estimate that in 2017, there were approximately 1.6 million high-risk alcohol users in Spain (1,200,000 men and 400,000 women) (Observatorio Español de las Drogas y las Adicciones, 2020).
At the organ level, the liver is by far most affected by alcohol abuse because it metabolises most of the ethanol consumed and produces a potentially toxic metabolite (acetaldehyde) as well as free radicals that cause liver damage (Cederbaum, 2012). However, alcohol use disorder (AUD), formerly known as alcohol dependence, is a systemic disease with an impact on a wide range of organs, some of which are less familiar to the general public. For instance, the immune, neurological, and cardiovascular systems can also be affected in patients who consume excessive amounts of alcohol. In addition, it has been shown that alcohol can be a carcinogenic agent; in fact, it has been associated with various types of cancer including liver, head and neck, oesophageal, and breast tumours, among others (Degenhardt et al., 2018).
The Spanish Network on Addictive Disorders (RTA in its Spanish initialism) was created in 2003, thanks to the Thematic Networks for Cooperative Research in Health (RETICS) programme funded by the Carlos III Health Institute. This scientific network currently consists of 18 research groups from different regions of Spain and is dedicated to expanding academic knowledge about substance abuse, its origins, and consequences. Within the RTA framework, the first multicentre study of Spanish patients with AUD seeking treatment for the first time (CohRTA study) was carried out in 2013 (Sanvisens et al., 2017) and to date, has enrolled over 900 patients and has a biobank of associated biological samples.
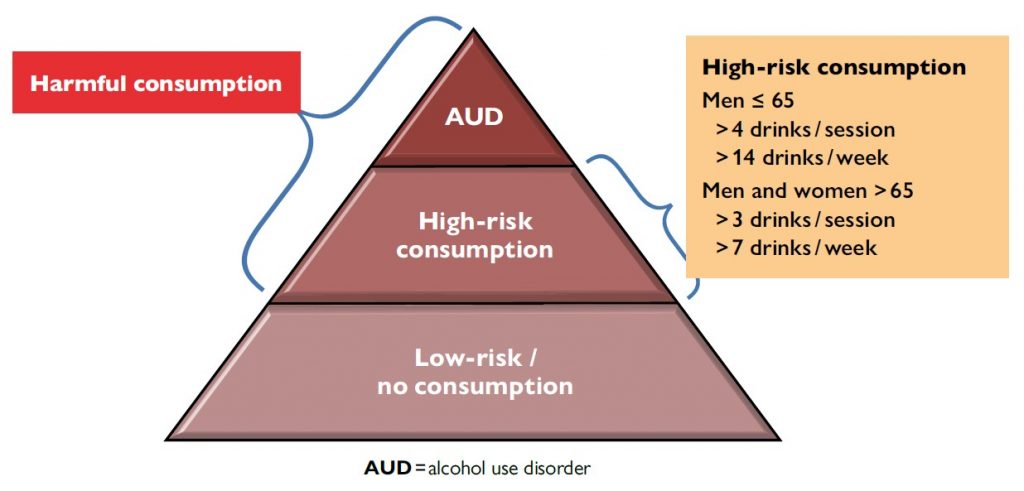
High-risk alcohol drinking patterns can increase the chance of negative consequences for drinkers and their environment. Different forms of excessive alcohol consumption can pose a health risk or cause significant harm to individuals. These include heavy weekly or daily drinking, acute episodes of alcohol intoxication, and binge drinking (consuming five or more alcoholic drinks in a short period of time). / Source: Adapted from Pace, A., & Samet, H. J. (2016). Annals of Internal Medicine, 164(7), ITC49-ITC64.
Immune system: discreet disorders
The immune system is very complex and is key to host defence against pathogens; it comprises two components: innate and adaptive immunity (Szabo & Saha, 2015). Heavy alcohol consumption predisposes individuals to infections such as bacterial pneumonia, tuberculosis, viral hepatitis, or human immunodeficiency virus (HIV), among others. In addition, patients who drink an excessive amount of alcohol are susceptible to developing serious complications (e.g., sepsis) during the course of an infection. The direct effects of alcohol on the immune system play a major role in infection pathogenesis, although other factors such as malnutrition, liver disease, and social vulnerability contribute to an increased risk of infection.
The deleterious effects of alcohol on the immune response will depend on the organ or system affected; the most extensively studied are the liver, lung, gastrointestinal tract, cardiovascular system, and nervous system. Furthermore, depending on the pattern of consumption (acute or chronic, regular or binge drinking), the effects on the immune response will differ.
Alcohol consumption may also promote the growth of Gram-negative bacteria in the gut, which can result in increased intestinal permeability and increased levels of lipopolysaccharides in peripheral blood. Lipopolysaccharides activate immune cells and their inflammatory response via cytokines and inflammatory mediators.
Innate immunity is the first line of host defence. It produces an immediate and non-specific response when exposed to any antigen and results in molecular and cellular activation to contain the infection. The binding between molecules and receptors precipitates a series of intracellular signals that results in the activation of the so-called transcription factors required to control gene expression. Once activated, these factors result in the production of a series of cytokines (interleukins [IL] 1 and 6, tumour necrosis factor α [TNF-α], and interferon [IFN]), chemokines, cell-adhesion molecules, and immunoreceptors, which promote the activation, migration, and recruitment of cells and effector molecules to the site of infection.
In contrast, adaptive immunity is a delayed, complex, and specific response requiring prior contact with the antigen, and can create an immunological memory. It has two main components: cellular and humoral.
«Alcohol use has been hegemonic among addictive substances throughout human history»
T and B lymphocytes are the two main cellular populations of adaptive immunity. An antigen can stimulate both cell receptors, but the vast majority of B lymphocytes require the assistance of helper T lymphocytes to become activated and produce specific antibodies. Therefore, the activation of naive T cells is considered an essential step in the adaptive response.
The humoral component consists of immunoglobulins produced by activated B-lymphocytes; both non-specific and specific antibodies can remove extracellular micro-organisms. Different types of immunoglobulins are produced at different times during an infection and in response to a wide variety of antigens.
Alcohol is an immunosuppressant that can affect all components of innate and adaptive immunity through direct or indirect toxicity mechanisms originating in ethanol metabolism. Notably, in addition to the impact on the risk of infections, defects in the immune response play an important role in the pathogenesis of alcoholic liver disease, acute pancreatitis, some types of cancer, atherosclerosis, and impaired wound healing.
Moreover, the structure and size of the ethanol molecule allow it to easily traverse cell membranes; therefore, the molecular and metabolic changes produced by ethanol molecules can alter all immune system cells, ultimately impacting their number, functioning, and survival, and leading to the system ageing prematurely (Zuluaga et al., 2020).
Neurological alterations: a classic presentation
Nervous system disorders associated with alcohol abuse are mainly derived from the direct toxic effect of ethanol and from nutritional disturbances but may also be secondary to the dysfunction of other organs, as in the case of hepatic encephalopathy (Rao & Topiwala, 2020).
«Alcohol use disorder is a systemic disease which affects a wide range of organs and psychological processes»
Sustained alcohol abuse can lead to alterations in multiple central and peripheral nervous system structures, resulting in a disproportionate loss of cerebral white matter, along with alterations in cognitive function, cerebellum, skeletal muscle, or peripheral nerves, among others.
Diseases that may be related to ethanol toxicity include dementia, cerebellar degeneration, and polyneuropathy. Cerebellar degeneration usually appears gradually over weeks or months but may also develop over years or begin with an acute episode. It usually starts with gait disturbances, characterised by weakness, or uncoordinated limb movement. Conversely, polyneuropathy occurs gradually and progressively, starting with impaired sensation and subsequently leading to alterations in motor and autonomic functions. It is generally symmetrical and mostly affects the lower extremities. Common symptoms include tingling, paraesthesia, dysesthesia, pain, weakness, and gait disturbances.
One of the most significant nutritional disturbances associated with AUD is thiamine deficiency. Wernicke’s encephalopathy is an acute neurological disease associated with this deficiency; clinically, it is characterised by the onset of mental confusion, ocular disturbances, and ataxia, as described by Carl Wernicke in 1881. Once identified, this condition responds to treatment with vitamin B1, but in its chronic form, known as Korsakoff’s syndrome, it evolves into irreversible psychosis or dementia. Thiamine deficiency causes brain damage, with the cerebellum being the most affected part of the brain. Several studies have described the prevalence of Wernicke’s encephalopathy at 0.8 % to 2.8 % of the general population and 12 % among patients with AUD. The mortality rate of patients with this disease is 17 %; however, contemporary research on this pathology and its prognosis is very scarce. In fact, there is probably a high percentage of undiagnosed Wernicke’s disease because of the difficulty in recognising its clinical manifestations, the absence of reliable biological markers, and the lack of detection of alcohol use. Of note, in 2012, the Working Group on Alcohol and Alcoholism of the Spanish Society of Internal Medicine promoted a multicentre study involving 21 Spanish hospitals, and successfully recorded one of the largest series of cases of this disease, with 434 patients (Chamorro et al., 2017).

Wernicke’s encephalopathy is an acute neurological disease associated with thiamine deficiency; clinically, it is characterised by the onset of mental confusion, ocular disturbances, and ataxia, as described by Carl Wernicke (on the left) in 1881. Once identified, this condition responds to treatment with vitamin B1, but in its chronic form, known as Korsakoff’s syndrome, it evolves into irreversible psychosis or dementia. Sergei Korsakoff (on the right) was the first person to associate mental symptoms and peripheral neuropathy with a single cause: the effects of alcohol abuse on the central nervous system. / Image source: US National Library of Medicine
Cardiovascular disease: the controversy continues
The general population is not generally aware that alcohol consumption may be associated with cardiovascular disease. Unlike classic risk factors such as smoking or hypercholesterolemia, excessive alcohol consumption goes somewhat more unnoticed as a preventable cause of cardiovascular damage. Moreover, numerous studies have reported the cardioprotective effect of moderate alcohol consumption and so, controversy is rife. In fact, the debate on the potential benefits of alcohol consumption dates back to the late 1970s, when The Lancet published an inverse association between alcohol consumption and coronary heart disease mortality.
he effect was attributed to the beneficial properties of moderate wine consumption (Leger et al., 1979). Four decades later, the results of a population-based study of nearly 600,000 individuals without cardiovascular disease from 83 cohorts in 19 countries were published in the same journal and concluded that regular consumption of one alcoholic drink per day linearly increases the risk of cerebrovascular disease, heart failure, and death from cardiovascular disease, except for acute myocardial infarction (Wood et al., 2018).
Beyond this protracted debate, the truth remains that alcohol abuse is the most common cause of nonischaemic dilated cardiomyopathy in the world. In Spain, the prevalence of alcoholic cardiomyopathy in patients with AUD is estimated to be 13 %, but to date, the time and amount of alcohol consumption required for this pathology to appear has still not been accurately defined. Alcoholic cardiomyopathy is characterised by asymptomatic left ventricular dilation and dysfunction and it is estimated that signs or symptoms do not emerge until at least 15 years of harmful drinking. This disease is indistinguishable from other forms of cardiomyopathy, hence the importance of considering alcohol consumption as a risk factor for cardiovascular disease. A preclinical form of alcoholic cardiomyopathy is the so-called holiday heart syndrome, characterised by the appearance of a cardiac arrhythmia (atrial fibrillation) after heavy drinking episodes during vacations.
Alcohol consumption, be it acute or chronic, may also be associated with high blood pressure and the development of heart rhythm problems or arrhythmias that may be clinically invisible.
The direct toxic action of ethanol takes place within myocardial cells; the enzyme aldehyde dehydrogenase catalyses the transformation of ethanol into acetaldehyde, which can concentrate in the myocardium and alter the functional and structural integrity of myocardiocytes. Other processes resulting from alcohol abuse, like oxidative stress, systemic inflammation, or intestinal permeability, may also play a role (García-Calvo et al., 2020).
Ongoing research is trying to determine the molecular mechanisms through which alcohol causes cardiac damage, although the existence of a genetic and/or epigenetic predisposition in certain individuals seems to be clear.
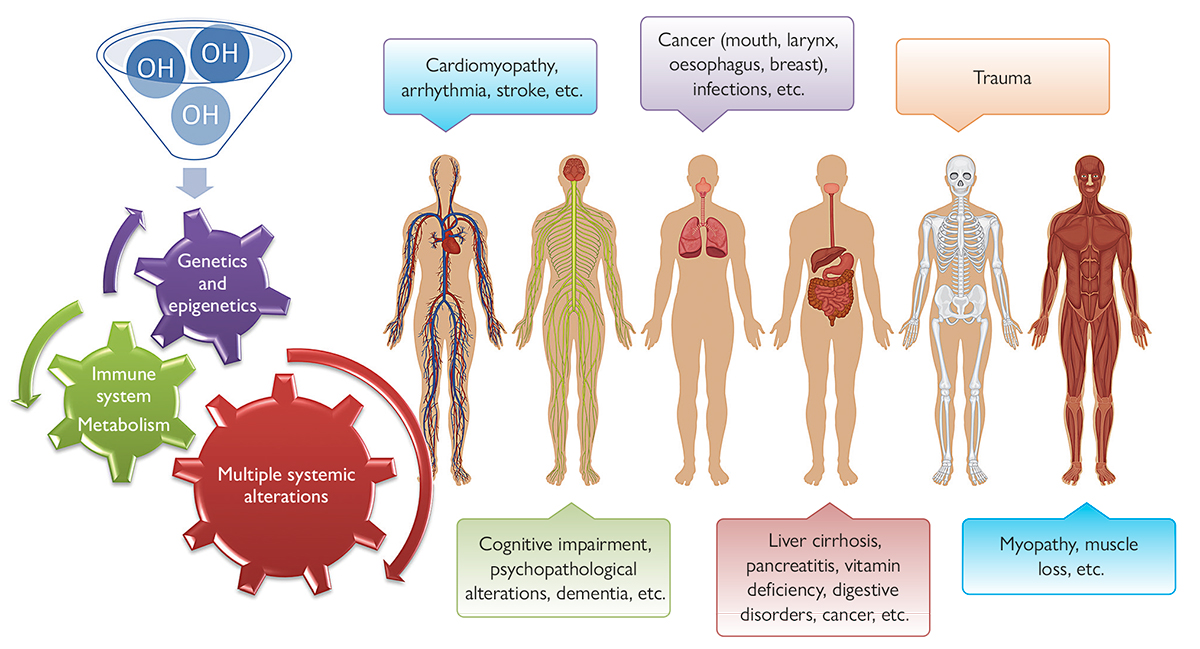
Disorders related to the use of alcohol – which, in broad terms, is an organic substance with an OH hydroxyl group – can cause a wide variety of organ conditions in the human body, some of which are not well known to the general population. While the liver is the organ most affected by alcohol abuse, our metabolism, as well as our immune, neurological, and cardiovascular systems, among others, can also be impacted resulting in the development of different diseases. In addition, both alcohol use disorder and its complications may have genetic (e.g., some genetic modifiers may be involved in ethanol metabolism) and epigenetic components, because changes in phenotypic expression caused by alcohol consumption may be passed on to the next generation. / Source: Authors, infographic created with Vecteezy
Genetics and epigenetics: emerging research
Over the years, it has been well established that both excessive alcohol consumption and its associated complications may have a genetic component. For example, there are genetic modifiers of neurotransmission, such as genes encoding the GABA receptor, i.e., the receptor for a neurotransmitter involved in neuron-to-neuron communication, or genetic modifiers of ethanol metabolism, in particular polymorphisms of enzymes involved in ethanol metabolism (Anstee et al., 2015).
It is also clear that DNA alone is not the only source of information transmission between generations. Grouped under the umbrella term epigenetics, the chemical modifications of DNA, chromatin, and non-coding RNA, are critical molecular processes that regulate gene expression.
Epigenetic alterations are defined as hereditary changes in gene expression, caused not by alterations in the DNA sequence, but by changes in the DNA structure. These are post-translational DNA methylation and histone modifications that change the structure and function of chromatin. More specifically, epigenetic inheritance can arise when these marks are not removed in germ cells and can therefore be passed on from one generation to the next, thus contributing to phenotypic diversity.
Diet, environmental toxicants, and stress have all been shown to alter epigenetic marks, and there is evidence that these «exposures» can cause transgenerational phenotypes that may involve epigenetic inheritance. The involvement of epigenetic inheritance in the transgenerational effects of alcohol is not well studied but could lead to significant advances in understanding vulnerability to AUD and its consequences (Berkel & Pandey, 2017).
Clearly, epigenetic changes, whether transient or permanent, play a fundamental role in the action of alcohol on different cellular processes and organ systems. Thus, understanding the exact nature of the way alcohol interacts with the epigenome could help to design better medications to treat a wide range of alcohol-related disorders and alcohol-induced organ damage.
Conclusions
UD is a systemic disease with serious health consequences. In Spain, the demand for treatment for alcohol abuse is growing. In fact, the number of patients entering treatment for alcohol abuse disorder has increased in recent years to become the leading cause of demand for treatment, well above that for cocaine and other substance use disorders. The loss of quality of life and health in these patients is clear, and prevention and harm reduction should be priorities in public health actions and deemed essential for the wellbeing of society.
New research projects focusing on the systemic complications of AUD and epigenetic alterations produced by this substance must be developed, but it is even more important to disseminate these results to society.
This work was partially funded by the Spanish Ministry of Science and Innovation, the Carlos III Health Institute, and ERDF funds (RD16/0017/0003, PI17/00174), as well as by the National Drug Plan of the Spanish Ministry of Health (PNSD 2018/020).
References
Anstee, Q. M., Daly, A. K., & Day, C. P. (2015). Genetics of alcoholic liver disease. Seminars in Liver Disease, 35(04), 361–374. https://doi.org/10.1055/s-0035-1567832
Berkel, T. D. M., & Pandey, S. C. (2017). Emerging role of epigenetic mechanisms in alcohol addiction. Alcoholism: Clinical and Experimental Research, 41, 666–680. https://doi.org/10.1111/acer.13338
Carrigan, M. A., Uryasev, O., Frye, C. B., Eckman, B. L., Myers, C. R., Hurley, T. D., & Benner, S. A. (2015). Hominids adapted to metabolize ethanol long before human-directed fermentation. Proceedings of the National Academy of Sciences of the United States of America, 112(2), 458–463. https://doi.org/10.1073/pnas.1404167111
Cederbaum, A. I. (2012). Alcohol metabolism. Clinics in Liver Disease, 16(4), 667–685. https://doi.org/10.1016/j.cld.2012.08.002
Chamorro, A. J., Rosón-Hernández, B., Medina-García, J.-A., Muga-Bustamante, R., Fernández-Solá, J., Martín-González, M.-C., Seco-Hernández, E., Novo-Veleiro, I., Suárez-Cuervo, C., Mateos-Díaz, A. M., Monte-Secades, R., Machado-Prieto, B., Puerta-Louro, R., Prada-González, C., Fernández-Rial, Á., Sabio-Repiso, P., Vázquez-Vigo, R., Antolí-Royo, A.-C., Gomila-Grange, A., … Laso, F.-J. (2017). Differences between alcoholic and nonalcoholic patients with Wernicke encephalopathy: A multicenter observational study. Mayo Clinic Proceedings, 92(6), 899–907. https://doi.org/10.1016/j.mayocp.2017.02.019
Degenhardt, L., Charlson, F., Ferrari, A., Santomauro, D., Erskine, H., Mantilla-Herrara, A., Whiteford, H., Leung, J., Naghavi, M., Griswold, M., Rehm, J., Hall, W., Sartorius, B., Scott, J., Vollset, S. E., Knsudse, A. K., Haro, J. M., Patton, G., Kopec, J., … Vos, T. (2018). The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. The Lancet Psychiatry, 5(12), 987–1012. https://doi.org/10.1016/S2215-0366(18)30337-7
García-Calvo, X., Bolao, F., Sanvisens, A., Zuluaga, P., Tor, J., Muga, R., & Fuster, D. (2020). Significance of markers of monocyte activation (CD163 and sCD14) and inflammation (IL-6) in patients admitted for alcohol use disorder treatment. Alcoholism: Clinical and Experimental Research, 44(1), 152–158. https://doi.org/10.1111/acer.14228
Leger, A. S. S., Cochrane, A. L., & Moore, F. (1979). Factors associated with cardiac mortality in developed countries with particular reference to the consumption of wine. The Lancet, 313(8124), 1017–1020. https://doi.org/10.1016/S0140-6736(79)92765-X
Observatorio Español de las Drogas y las Adicciones. (2020). INFORME 2020 Alcohol, tabaco y drogas ilegales en España. https://pnsd.sanidad.gob.es/
Rao, R., & Topiwala, A. (2020). Alcohol use disorders and the brain. Addiction, 115(8), 1580–1589. https://doi.org/10.1111/add.15023
Sanvisens, A., Zuluaga, P., Rivas, I., Rubio, G., Gual, A., Torrens, M., Short, A., Álvarez, F. J., Tor, J. Farré, M., Rodríguez de Fonseca, F., & Muga, R. (2017). Patients with alcohol use disorder: initial results from a prospective multicenter registry in the Spanish Network on Addiction Disorders. CohRTA Study. Adicciones, 30(4), 931. https://doi.org/10.20882/adicciones.931
Szabo, G., & Saha, B. (2015). Alcohol’s effect on host defense. Alcohol Research: Current Reviews, 37(2), 159–170. https://pubmed.ncbi.nlm.nih.gov/26695755/
Wood, A. M., Kaptoge, S., Butterworth, A., Willeit, P., Warnakula, S., Bolton, T., Paige, E., Paul, D. S., Sweeting, M., Burgess, S., Bell, S., Astle, W., Stevens, D., Koulman, A., Selmer, R. M., Verschuren, W. M. M., Sato, S., Njølstad, I., Woodward, M., … Danesh, J. (2018). Risk thresholds for alcohol consumption: Combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. The Lancet, 391(10129), 1513–1523. https://doi.org/10.1016/S0140-6736(18)30134-X
Zuluaga, P., Sanvisens, A., Teniente-Serra, A., El Ars, O., Fuster, D., Quirant-Sánchez, B., Martínez-Cáceres, E., & Muga, R. (2020). Loss of naive T lymphocytes is associated with advanced liver fibrosis in alcohol use disorder. Drug and Alcohol Dependence, 213, 108046. https://doi.org/10.1016/j.drugalcdep.2020.108046





