Re-imagining One Health
A perspective from social science

One Health is a framework focusing on the dynamic intersections between humans, animals, and ecosystems regarding health systems and practices. As human decisions and actions are the locus of One Health challenges, it is critical to understand how people perceive and act on these connections. Fundamentally, the literature in this area is based in the natural and health sciences; further efforts are still necessary to fully realize the potential of bringing social research squarely into One Health. We suggest several areas of scholarship that could move this effort forward.
Keywords: One Health, interdisciplinary framework, risk, social sciences, zoonoses.
Although no one universally agreed-upon definition exists, One Health is essentially an area of study that focuses on the dynamic intersections among humans, animals, and ecosystems regarding health systems and practices (e.g., Soares, 2020). The goal of One Health is improving overall health outcomes through synergistic activities among seemingly disparate yet interconnected communities. Some areas of work include food safety, the control of zoonoses, and reducing antibiotic resistance. This essay presents contributions of social science to our understanding of One Health.
Fundamental social issues
Lapinski et al. (2015) suggested three key ways social science writ large could contribute to One Health research and practice: a) examine how humans contextualize their own health within animal and ecosystem health; b) study the ways in which information and communication can improve One Health decisions and outcomes; and c) identify the key characteristics of new and emerging communication technologies and how and when they are used and can be used globally for One Health.
These ideas were high-level and meant to generate research questions and hypotheses on core One Health issues like zoonotic and emerging infectious disease, climate change, and anti-microbial resistance (AMR), but also to push the envelope on other issues (e.g., water protection or conservation, land use decisions, deforestation, animal husbandry practices, etc.). Here we briefly describe these three broad issues following Lapinski et al. (2015) as well as other relevant literature on the matter. Figure 1 depicts the case of the spread of antimicrobial resistant pathogens in human populations and provides example social science research directions.
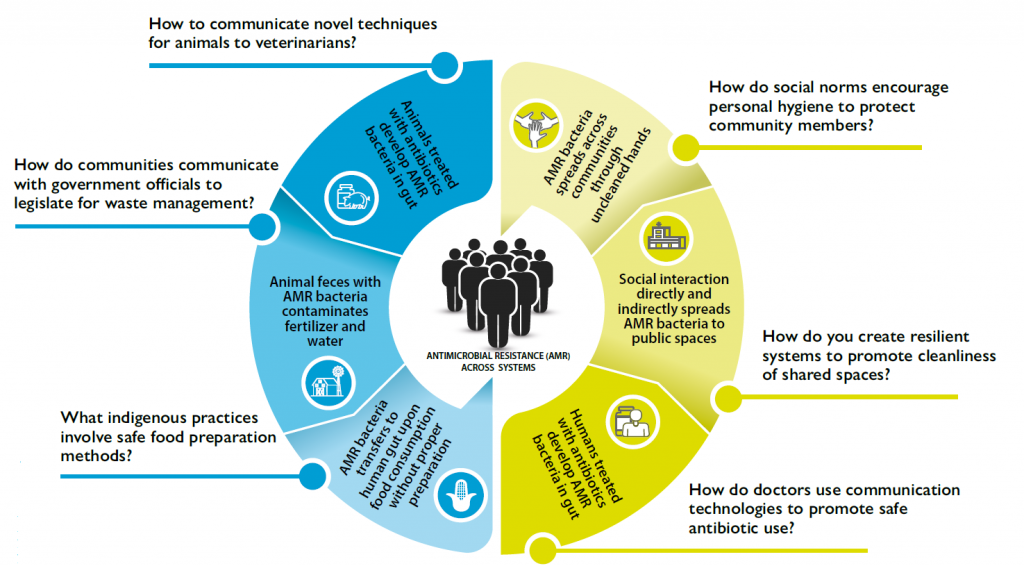
Figure 1. Antimicrobial resistant pathogen spread and example social science research questions. / Source: Clare Grall (2020). This work is licensed under a CC BY 4.0 license.
How do people perceive and act on One Health?
As human decisions and actions are the locus of One Health challenges, it is critical to understand how people perceive and act on these connections. Fundamentally, this is a question of having formative social data and community engagement to understand how people are likely to shape, contribute, or react to system changes or interventions. Understanding this is premised on a systems approach to individual decisions about One Health issues; this requires acknowledging the complexity of factors driving what people will do and how that action is shaped by, or will shape, the world around them (see Partelow, 2018; Stokols, 1996).
There is applied research which uses this approach, including the 28 country PREDICT-2 (Saylors et al., 2021), a project for the global surveillance for pathogens that can spillover from animal hosts to people. It uses behavioral risk and sociocultural data to understand zoonotic disease. The project examined behaviors, attitudes, knowledge, demographics, and health history on disease emergence and transmission. It focused on people at the human-animal-ecosystem interface leading to a culturally targeted intervention resource. Similarly, Beall et al. (2021) take a cultural cognition approach to the zoonotic linkages between the wildlife trade, the ecology, and the emergence of Covid-19 to design and test messages about these issues. Yet rarely is social or behavioural theory at the center of efforts to understand One Health relationships; doing so would add to our ability to predict and explain outcomes.
What is the role of communication and information in One Health decision-making?
A better understanding of the effects of human interactions (both mediated and non-mediated) and strategically designed interventions will help to inform how to approach One Health problems. Research on the effects and processes of information and communication is found in several disciplines; only rarely do these studies take an explicitly One Health approach but there is literature in antimicrobial resistance which is relevant.
In the context of AMR, research efforts exist at all systemic levels (see Smith et al., 2015). Some of this focuses on changing the practices of human and animal health providers and clients through strategic communication. Systematic reviews indicate that for human health, use of antibiotics can be reduced through patient or physician education and understanding the decisions made by prescribing physicians and their interactions with clients (Ranjit et al., 2008; Rogers et al., 2019). In animal health, changes to the policy environment, veterinarian practices, and animal owner behaviour can reduce use of antibiotics and antimicrobials. And, recently, calls to shift the focus of AMR research to understand social norms suggest new directions for research (Hernando-Amando et al., 2020).
How is communication technology used and useful in One Health?
The final issue raised in Lapinski et al. (2015) was a call to focus on the role of communication technology in One Health. Communication technology is fundamental to the ways people experience and interact with the world and plays a central role in how One Health challenges unfold and are addressed. One example is the spread of the zoonotic SARS-CoV-2 misinformation on social media, its influence on human behaviors, and ultimately on the trajectory of the pandemic.
Examples of the ways in which communication technologies can be useful in One Health include prediction and surveillance of disease, documenting and intervening in illegal destruction of ecosystems or poaching and trading of wildlife, determining trends in human behavior and cognitions through analysis of social media data, and the use of applications and serious games to promote risk reduction or information seeking. The research and application of the function of communication technologies for One Health will evolve as new technologies emerge and represents a novel area of One Health inquiry.
One Health, crisis, and resilience
Zika, Ebola, chemical spills and contamination, and natural hazard events impacting the human-built system have all been framed within the One Health perspective. One Health focuses attention on interdependencies and the ways changes, sometimes minor, may impact the operation of other dependent systems creating health risks. This sensitive dependence on initial conditions in complex, non-linear systems is well documented as a source of substantial threats, disruptions, and crises that create significant and widespread harm.
An interdisciplinary conceptual framework for understanding the operations of complex systems and interdependent groups of systems is resilience (Bené et al., 2018; Bourbeau, 2018). Resilience was extended from ecological studies and systems theory to understand physical systems, people, environments, and their interactions. The concept concerns the capacity and processes whereby systems can anticipate, avoid, respond, and bounce back from threats imposed by serious disruptions, crises, and disasters.
Resilience is an attribute of systems as well as the ways systems interact, communicate with, and receive mutual support from other interdependent systems. Resilience can also occur at the individual, organizational, community, and national levels. In the Flint (Michigan, USA) Water Crisis, for example, the health of individual community members was impacted by the water from the Flint River that was not treated effectively by the municipal water system. This was enabled by a political system that disenfranchised some poor and minority communities and compounded by underlying health disparities. Interdependent natural, political, social, and engineered systems were all factors in this health crisis (Nowling & Seeger, 2020). The community lacked the capacity to anticipate, avoid, and respond to the crisis. In other words, it lacked resilience. The public health crisis of the Zika virus involved the intersection of behavioral and climatic factors and the natural and human built environment. Increasing global populations, more mosquitos, increased urbanization, and increasing global transportation of commercial goods and people likely facilitated the shift in Zika from a rare disorder found in parts of Africa to a major global health threat.
A variety of resilience perspectives have been proposed. The four R model of robustness, redundancy, resourcefulness, and rapidity offers a systems dynamic approach to resilience (Florin & Linkov, 2016). Robustness concerns the ability of systems to resist stress without suffering major disruption. Fragile ecosystems may suffer serious damage from even minor disruptions. Redundancy is the extent to which systems continue functionality even in the event of disruptions or damages. Many natural disasters, such as the 2005 Hurricane Katrina disaster, the 2012 floods in Western Europe, and the 2011 Joplin, Missouri tornadoes, create significant system disruption. Resourcefulness concerns the capacity to anticipate problems and mobilize resources to avoid disruption or reduce its impact. Rapidity is the capacity to respond to threats in a timely manner to contain losses and limit damage. Many infectious disease outbreaks, including Covid-19, were not contained because of inadequate resourcefulness and rapidity of response.
Systemic disruptions, crises, and disasters have profound impacts on human health. The 1918 Spanish Flu pandemic caused as many as 50 million death world-wide (Overby et al., 2005). WHO estimates that foodborne illness causes 600 million cases annually and leads to 420,000 deaths, 30 % among children under 5 years of age. The 2004 Indian Ocean Tsunami killed an estimated 227,898 people in 14 countries and devastated economies (Ahmadun et al., 2020). In addition to deaths and hospitalizations, disruptions create social, mental, and economic harm, both in the short and long term.
These systemic disruptions are a function of a wide array of established and emerging hazards, including emerging and re-emerging infectious diseases. Chemical spills and contamination including petroleum, heavy metals, per- and polyfluoroalkyl substances, and radiological events cause illness, impact natural systems and agriculture, and cause social and economic disruption. Climate change is expected to create widespread and profound disruption to ecosystems, the human-built environment, and social and economic systems, displacing populations, fundamentally disrupting economies, and altering agricultural practices. Extreme weather events, frequent flooding, hurricanes, tornadoes, and droughts are predicted to become more common. Climate change can also create secondary disruptions to ecosystems in ways that promote the emergence and reemergence of infectious disease.
These and other kinds of serious disruptions of interdependent systems can be mitigated by a focus on system resilience. This includes understanding interdependencies, anticipating sources of disruption, and incorporating them into planning; zoonotic disease connected to the food system is a case where building resilience is critical.
Zoonoses and risk
Zoonotic diseases are often exchanged among agricultural workers and animals and may then spread broadly. Salmonella transmitted via animals to humans is one example. There is growing concern among scientists about exponential increases in mosquito-borne viruses and infectious diseases being spread by animals today as the Earth warms. Some agencies, such as the United States Geological Survey’s Climate Adaptation Science Centers (USGS-CASCs), are currently examining climate change impacts on fish, wildlife, and ecosystems and preparing research-based state wildlife action plans.

There is a growing concern among scientists about exponential increases in mosquito-borne viruses and infectious diseases being spread by animals today as the Earth warms. / James Gathany – CDC
The global impact of these complex interconnections was made apparent when SARS-CoV-2 outbreaks among employees forced U.S. meatpacking plants to temporarily shut down, leading to a plethora of implications. Although these industries had robust biosecurity plans in place to impede the spread of disease among animals, Covid-19 caught the industry unprepared and resulted in millions of animals being destroyed (Economic Research Service, 2021). Another example comes from swine industry as a success story in mitigating the spread of porcine epidemic diarrhea virus (PEDV) – a novel virus to the United States at the time (2014) – in a matter of months. Lessons learned from the successful integration of agricultural biosecurity quickly quelled the staggering losses of nearly 100,000 baby piglets each week.
One approach to addressing such complex risks is to form global communities of practice. These are «groups of people, networks, or institutions sharing interests, exchanging information or discussing ideas on a specific topic of common interest by interacting on an ongoing basis» (Pan American Health Organization, 2015). The community of practice perspective can be a method for implementing the One Health approach because representatives from myriad subnetworks and disciplines play a role in responding effectively to crises. In the case of the U.S. meatpacking industry during the SARS-CoV-2 pandemic, the biosecurity practices that had been widely effective during the PEDV outbreak were negated by the swine industry’s failure to account for the risks to human health and cascading impacts on the industry. Close working conditions within processing plants contributed to the spread of SARS-CoV-2. Planning for similar crises includes maintaining animal biosecurity while creating alternatives in plant design for workers.
Responding to such crises effectively requires exceptional collaboration. Collaborations can, however, also serve a proactive purpose. Courtenay et al. (2015) describe a case where physicians and veterinarians started making joint rounds, observing cases where failing animal health was linked to human health and vice versa. Hueston and colleagues (2013) identify several promising communication strategies for promoting One Health. First, they emphasize the value of narratives or success stories. Stories featuring interdisciplinary interaction and successful individual outcomes are quite compelling. Second, they suggest recruiting individuals who have seen the success of One Health first-hand to serve as spokespersons. Third, a commitment to expanding and solidifying interdisciplinary partnerships is essential. Finally, they advocate a global approach in promoting One Health. Importantly, the value of One Health should be directly observable to stakeholders.
What’s next for One Health social science research?
Despite the numerous advances, there are many exciting issues that remain unexplored. Fundamentally, the One Health literature is based in the natural and health sciences; efforts are still nascent to fully realize the potential of bringing social research squarely into One Health. We suggest several areas of scholarship that could move this effort forward: 1) Replication of studies of basic social processes in One Health contexts and building theory about the ways in which One Health challenges are similar and different from other issues. 2) Development and testing of new theory about One Health and social dynamics, including theorizing resilient One Health systems. 3) Examining Indigenous conceptualizations of One Health, including for those people living at the intersection of the three forms of health to inform global One Health theory and practice. 4) A greater focus on the role of interpersonal and social relationships in shaping human response to One Health issues. 5) Continued efforts to look at the ways in which interactions with and information from animals and ecosystems shape human experience, health, and well-being (and vice versa). 6) Translation and dissemination of findings of studies of health which can contribute to human, animal, and ecosystem health in synergistic ways.
These directions and others provide an important agenda for future research on and application of One Health. It is hoped that bringing social science more directly into the One Health mix will help fulfill the promise of this significant integration. The successes noted above indicate the value of One Health and the need to make meaningful moves to avoid the imminent challenges facing our world.
References
Ahmadun, F.-R., Wong, M. M. R., & Said, A. M. (2020). Consequences of the 2004 Indian ocean tsunami in Malaysia. Safety Science, 121, 619–631. https://doi.org/10.1016/j.ssci.2019.05.016
Beall, J. M., Casola, W. R., Peterson, M. N., Larson, L. R., Carr, W. A., Seekamp, E., Stevenson, K. T., & Jackson, S. B. (2021). Cultural cognition and ideological framing influence communication about zoonotic disease in the era of Covid-19. Frontiers in Communication, 6, 645–692. https://doi.org/10.3389/fcomm.2021.645692
Béné, C., Mehta, L., McGranahan, G., Cannon, T., Gupte, J., & Tanner, T. (2018). Resilience as a policy narrative: Potentials and limits in the context of urban planning. Climate and Development, 10(2), 116–133. https://doi.org/10.1080/17565529.2017.1301868
Bourbeau, P. (2018). A genealogy of resilience. International Political Sociology, 12(1), 19−35. https://doi.org/10.1093/ips/olx026
Courtenay, M., Sweeney, J., Zielinska, P., Brown Blake, S., & La Ragione, R. (2015). One Health: An opportunity for an interprofessional approach to healthcare. Journal of Interprofessional Care, 29(6), 641–642. https://doi.org/10.3109/13561820.2015.1041584
Economic Research Service. (2021). The meatpacking industry in rural America during the Covid-19 pandemic. https://www.ers.usda.gov/covid-19/rural-america/meatpacking-industry
Florin, M.-V., & Linkov, I. (Eds.). (2016). IRGC resource guide on resilience. EPFL International Risk Governance Center. https://doi.org/10.5075/epfl-irgc-228206
Hernando-Amado, S., Coque, T. M., Baquero, F., & Martínez, J. L. (2020). Antibiotic resistance: Moving from individual health norms to social norms in one health and global health. Frontiers in Microbiology, 11, 1914. https://doi.org/10.3389/fmicb.2020.01914
Hueston, W., Appert, J., Denny, T., King, L., Umber, J., & Valeri, L. (2013). Assessing global adoption of one health approaches. EcoHealth, 10(3), 228–233. https://doi.org/10.1007/s10393-013-0851-5
Lapinski, M. K., Funk, J. A., & Moccia, L. T. (2015). Recommendations for the role of social science research in One Health. Social Science & Medicine, 129, 51–60. https://doi.org/10.1016/j.socscimed.2014.09.048
Nowling, W. D., & Seeger, M. W. (2020). Sensemaking and crisis revisited: The failure of sensemaking during the Flint water crisis. Journal of Applied Communication Research, 48(2), 270–289. https://doi.org/10.1080/00909882.2020.1734224
Overby, J., Rayburn, M., Wyld, D. C., & Hammond, K. (2005). Looming cognition for global competition: The approaching avian influenza pandemic. Asia Pacific Journal of Marketing and Logistics, 17(2), 17–30. https://doi.org/10.1108/13555850510672322
Pan American Health Organization. (2015). Building communities of practice. https://iris.paho.org/handle/10665.2/35000
Partelow, S. (2018). A review of the social-ecological systems framework: Applications, methods, modifications, and challenges. Ecology and Society, 23(4), 36. https://doi.org/10.5751/ES-10594-230436
Ranji, S. R., Steinman, M. A., Shojania K. G., & Gonzales, R. (2008). Interventions to reduce unnecessary antibiotic prescribing: A systematic review and quantitative analysis. Medical Care, 46(8), 847–862. https://doi.org/10.1097/MLR.0b013e318178eabd
Rogers Van Katwyk, S., Grimshaw, J. M., Nkangu, M., Nagi, R., Mendelson, M., Taljaard, M., & Hoffman, S. J. (2019). Government policy interventions to reduce human antimicrobial use: A systematic review and evidence map. PLOS Medicine, 16(6), e1002819. https://doi.org/10.1371/journal.pmed.1002819
Saylors, K., Wolking, D. J., Hagan, E., Martinez, S., Francisco, L., Euren, J., Olson, S. H., Miller, M., Fine, A. E., Thanh, N. N. T., Minh, P. T., Kalengkongan, J. D., PREDICT Consortium, Kusumaningrum, T., Latinne, A., Pamungkas, J., Safari, D., Saputro, S., Bamba, D., … Mazet, J. A. (2021). Socializing One Health: An innovative strategy to investigate social and behavioral risks of emerging viral threats. One Health Outlook, 3, 11. https://doi.org/10.1186/s42522-021-00036-9
Sellnow, T. L., Parker, J. S., Sellnow, D. D., Littlefield, R. S., & Helsel, E. M., Getchell, M. C., Smith, J. M., & Merrill, S. C. (2017). Improving biosecurity through instructional crisis communication: Lessons learned from the PEDv outbreak. Journal of Applied Communications, 101(4). https://doi.org/10.4148/1051-0834.1298
Smith, R. A., M’ikanatha, N. M., & Read, A. F. (2015) Antibiotic resistance: A primer and call to action. Health Communication, 30(3), 309–314. https://doi.org/10.1080/10410236.2014.943634
Soares, A. (2020). William Karesh: Championing «One Health». Bulletin of the World Health Organization, 98(10), 652–653. https://doi.org/10.2471/BLT.20.031020
Stokols, D. (1996). Translating social ecological theory into guidelines for community health promotion. American Journal of Health Promotion, 10(4), 282–298. https://doi.org/10.4278/0890-1171-10.4.282