Breast cancer today
Advances in breast cancer epidemiology

ABSTRACT
Breast cancer is a health problem affecting women worldwide, and is so prevalent that for most of us it calls to mind the face of a relative, friend or acquaintance. Here we discuss the current situation of the disease around the world, with special reference to Spain, as well as the main risk factors.
Keywords: breast cancer, incidence, mortality, determinants.
BREAST CANCER AROUND THE WORLD
According to estimates by the International Agency for Research on Cancer (IARC), annually 1.44 million cases are diagnosed worldwide, half of which correspond to women from developing countries. In Europe more than 450,000 new cases are diagnosed each year. Geographic differences are less marked than a few decades ago, but there is a clear geographical pattern with higher incidence in the United States, Europe and Australia (Ferlay et al., 2010).
The twentieth century witnessed a rise in breast cancer worldwide; however, at the beginning of the 21st century there was a decrease in the United States and many other developed countries. This decrease corresponded primarily to women over 50, and was related to a decline in the use of hormone replacement therapy in postmenopausal women.
«Like most tumours, the frequency of this type of cancer increases exponentially with age, descending after menopause due to a decrease in hormone levels»
Breast cancer incidence in Spain is lower than in neighbouring countries, with adjusted rates of 61 cases per 100,000 women a year, while the European Union average is 77 per 100,000. Changes in Spanish women’s reproductive and social behaviour underlie the sharp increase in breast cancer over recent decades. In the 1990s, population screening programmes throughout Spain contributed to an increase in detected cases and a subsequent decline in our country at the beginning of this century. The regions that implemented screening earlier on experienced a drop in the number of cases detected once the susceptible population had been screened; the number of cases levelled off or even increased again later. Every year 27,000 new cases of breast cancer are diagnosed in Spanish women (Sánchez et al. 2010).
Thanks to early diagnosis and therapeutic advances, mortality began to decrease in the developed world in the 1990s. In Spain, cancer mortality has decreased at a rate of 2% annually since 1992. Currently, breast-cancer related deaths (6,280 in 2010) account for 3.4% of female mortality in our country (Pollán et al., 2009).
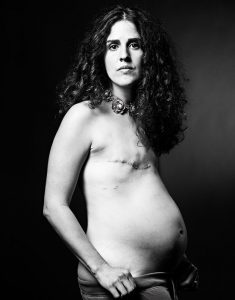
Pregnancy has a dual effect in the short and long term: on the one hand, pregnancy increases the level of circulating hormones, which is a risk factor in itself; on the other, completion of pregnancy leads to mammary gland maturation. The three pictures that illustrate this article belong to David Jay’s The SCAR Project which intends to show cancer free from artificial ornaments. /Images courtesy of David Jay/The SCAR Project (www.thescarproject.org)
MAJOR RISK FACTORS
Like most tumours, the frequency of this type of cancer increases exponentially with age, descending after menopause due to a decrease in hormone levels, as it is a hormone-dependent tumour (Colditz et al., 2006).
Hormonal and reproductive factor
Early menstrual onset – or menarche – and late menopause imply a greater exposure to oestrogen during a lifetime, thus increasing the incidence of hormone-related tumours. Late first pregnancy delays mammary gland maturation, again increasing the risk of developing breast cancer. Pregnancy has a dual effect in the short and long term: on the one hand, pregnancy increases the level of circulating hormones, which is a risk factor in itself; on the other, completion of pregnancy leads to mammary gland maturation. Childless women have a lower incidence of this tumour at a young age, and in general the risk in childless women is lower than in women who have their first baby later in life. Also, having many children and early ovariectomy are protective factors.
Concentrations of oestrogen and testosterone in blood are positively correlated with tumour frequency. Blood concentrations of insulin-like growth factor I (IGF-1) – also called somatomedin C – are positively correlated with tumour incidence (Key et al., 2010).
Oral contraceptives increase breast-cancer risk in young women but this risk disappears after suspending treatment, thus the overall effect is small. Hormone replacement therapy has a more significant effect, as it is prescribed at a time of life when tumour incidence is more common. Combination therapy, long-term treatment (fi ve years or more) and starting treatment during or immediately after menopause all increase the risk.
Family History and Genetic Susceptibility
A first-degree relative with breast cancer doubles the risk, showing the contribution of genetic factors. Indeed, numerous cases of breast cancer within the same family are sometimes due to high-impact or high-penetrance mutations. The main genes involved are BRCA1 and BRCA2, P523 and PTEN. Also genes CHEK2, BRIP1 and PALB2 are described as having moderate penetrance.
In most cases, genetic susceptibility is determined by the most common variant whose effect is modest and which, together, give rise to individual susceptibility. Large-scale studies are helping to identify a greater number of variants, as breast cancer is a complex disease due to the interaction between genetic and environmental factors.
«A first-degree relative with breast cancer doubles the risk, and numerous cases of breast cancer within the same family are often due to high-impact mutations»
Prenatal Risk Factors
Birth weight and advanced maternal age increase the risk of developing this tumour, refl ecting the effect of intrauterine hormone exposure. The height of adult women is considered to be a global marker of genetic, hormonal and nutritional factors that correlate positively with the incidence of breast cancer, as exposure to growth factors is considered to be greater.
Constitution of breast tissue: mammographic density
Mammographic imaging identifies the fibrous glandular tissue of the breast as a «light-coloured dense zone» against the dark-coloured fat. High mammographic density is one of the most important risk markers. Mammographic density depends on genetic susceptibility, but is also modulated by hormonal and reproductive factors. Clinical, genetic and epidemiological studies use mammographic density as a phenotypic marker of risk.
Personal History
Benign breast disease increases the risk of developing malignancy, particularly if accompanied by atypical hyperplasia. Ductal carcinoma in situ is a pre-invasive malignancy, whereas lobular carcinoma in situ is a precursor.
Type 2 diabetes and metabolic syndrome also increase breast cancer risk, partially due to obesity, which is associated with the aforementioned syndromes and is a risk factor in itself.
Obesity, Physical Activity and Dietary Factors
Obesity and weight gain in adulthood increase postmenopausal women’s risk of developing breast cancer as adipose tissue is a main oestrogen source. Conversely, physical activity acts as a protective factor.
Diet includes carcinogenic and anticancer substances. It is diffi cult to isolate the effect of a single nutrient, which explains why there is a lack of information regarding dietary factors that are clearly associated with breast cancer. In fact, alcohol consumption is the only clear diet-related risk factor. Sugar and rapidly absorbed carbohydrates may increase risk by increasing levels of insulin and IGF-1. The results of studies on fat intake are also mixed, polyunsaturated fatty acids and trans fats found in processed foods containing hydrogenated oils (margarine, industrial bakery products) would appear to increase the risk, while high omega-3 intake and consumption of olive oil would seem to exert a protective effect. Meat consumption also increases the risk, while fi bre intake decreases it.
Soy and other foods containing compounds with weak oestrogenic activity may interfere with the action and metabolism of endogenous oestrogens. Experimental and epidemiological studies provide somewhat contradictory results as to their influence on breast cancer risk, with a protective effect observed only in Asian women with very high consumption levels during childhood and adolescence.

Images courtesy of David Jay/The SCAR Project (www.thescarproject.org)
Experimental studies have shown that vitamin D inhibits the growth of tumour cells. Vitamin D concentrations depend on intake and sun exposure. Several studies suggest a protective effect, but so far results are not consistent. Folic acid participates in DNA synthesis and metabolism. Some population studies into low folic acid intake have shown an inverse relationship between folate levels and breast cancer incidence.
The study of «dietary patterns» is an alternative way to investigate the influence of diet. In this respect, unhealthy Western-type dietary patterns (high intake of meat, processed foods high in sugars and saturated and trans fats) increase the frequency of breast cancer, while a healthy diet (Mediterranean-type diet with high consumption of fruit, vegetables, fish and olive oil) would appear to reduce the risk.
Other Risk Factors: Environmental and Occupational Factors
Ionizing radiation can trigger breast cancer if exposure occurs in the first years of life, adolescence or pregnancy, when the mammary gland is developing. Ionizing radiation sources include X-rays and radiation therapy.
Studies in laboratory animals have identified more than 200 mammary carcinogens, but evidence in humans is scarcer, and the risk attributable to certain pesticides, solvents and endocrine disruptors is not sufficiently established.
«Obesity and weight gain in adulthood increase postmenopausal women’s risk of developing breast cancer, whereas physical activity is a protective factor»
Regarding occupational factors, higher incidence of breast cancer is recorded in secretaries, teachers, health-care workers, workers in the chemical and pharmaceutical industries, telephonists and hairdressers. People who do night shifts suffer disturbances in their circadian rhythm, which can mean melatonin secretion is deficient or lacking. Studies in experimental animal models support a relationship between circadian rhythm disruption and increased breast cancer; however, human evidence remains limited (Pollán, 2001).
WHAT CAN WE DO TO REDUCE THE RISK?
Reproductive factors are not easy to change. Fertility in Spain has decreased and women have their first baby at a later age. Although certain social policies can help to boost the birth rate, it is unrealistic to propose a radical change in reproductive patterns, which are subject to our current social and professional environment. Also, in Spain, as in other developed countries, the age of menarche is increasingly earlier.

World breast cancer distribution. Incidence rates adjusted for age: cases per 100.000 women-year. / Source: Ferlay et al., 2010
Nonetheless, there are more easily controlled factors. For instance, adults should avoid becoming obese and should take regular exercise, also avoiding or reducing alcohol consumption can contribute to preventing breast cancer and other diseases. Regarding specific dietary recommendations, although there is not enough evidence yet, it seems sensible to propose a reduction in the consumption of red meat, animal fats, processed foods and foods high in sugar, while encouraging the consumption of fibre, fi sh oil and virgin olive oil. This message is especially relevant to younger women, for whom worsening dietary patterns have been observed. Obesity is a growing problem worldwide. In Spain, 28% of women attending breast-cancer screening centres are obese.
All Spanish regions have population-screening programmes to diagnose breast cancer early, as recommended by European guidelines. These programmes aim to detect tumours in the early stages, thus improving therapeutic options and long-term prognosis.
Bibliography
Colditz, G. A. et al., 2006. «Breast Cancer». In Schottenfeld. D., & J. F. Fraumeni (eds.). Cancer Epidemiology and Prevention. 3 ed. Oxford University Press. New York.
Ferlay, J. et al., 2010. Globocan 2008, Cancer Incidence and Mortality Worldwide. International Agency for Research on Cancer. Lyon.
Key, T. J. et al., 2010. «Insulin-like Growth Factor 1 (IGF1), IGF Binding Protein 3 (IGFBP3), and Breast Cancer Risk: Pooled Individual Data Analysis of 17 Prospective Studies». The Lancet Oncology, 11(6): 530-542. DOI: <10.1016/S1470-2045(10)70095-4>.
Pollan, M., 2001. «Breast Cancer in Women and Occupation. A Review of the Evidence». Gaceta Sanitaria, 15(4): 3-22.
Pollan, M. et al., 2009. «Recent Changes in Breast Cancer Incidence in Spain, 1980-2004». Journal of the National Cancer Institute, 101(22): 1584-1591. DOI: <10.1093/jnci/djp358>.
Sánchez, M. J. et al., 2010. «Cancer Incidence and Mortality in Spain: Estimates and Projections for the Period 1981-2012». Annals of Oncology, 21(3): 30-36. DOI: <10.1093/annonc/mdq090>.





